| 
This booklet is aimed at men who are troubled by Lower Urinary Tract Symptoms (LUTS).
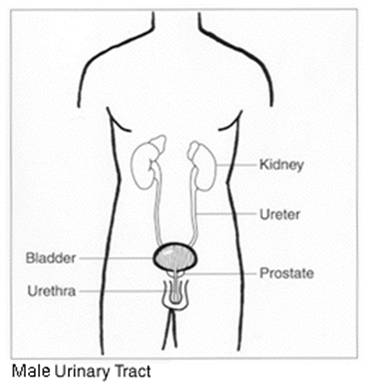
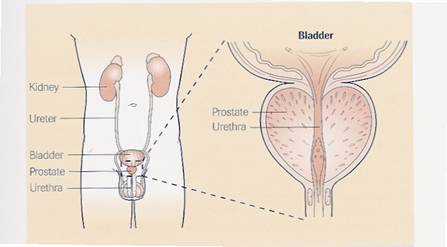
Doctors use the term ‘Lower urinary tract symptoms’ (or LUTS) to describe the problems they believe are related to the working of the bladder (which holds urine) and the urethra (the tube from the bladder to outside) through which urine passes when we pee/urinate.
There are many causes of these symptoms and investigation will allow us to determine the cause and the most appropriate treatment.
Prostatic enlargement which occurs because of benign prostatic hyperplasia (BPH) is a major cause of LUTS, as a result of obstruction at the exit of the bladder.
Other urological conditions such as a tight or enlarged bladder neck, an unstable bladder, or a narrowing in the urethra known as a ‘stricture’ may cause similar symptoms.
Not all LUTS are caused by a urological condition and other possibilities could involve cardiac, renal or neurological abnormalities.
We have two aims:
- To establish a diagnosis and to provide information about your symptoms and the treatment options available.

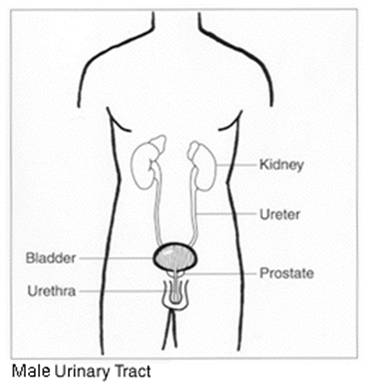
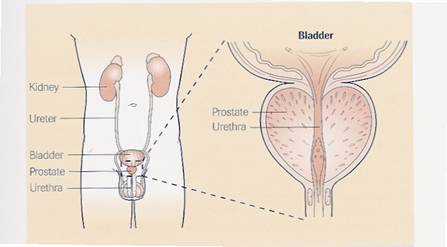
The prostate is a small gland, about the size of a walnut, which lies just below the bladder and is only present in men.
At present, Doctors do not fully understand all functions of the prostate. However, one of its main roles is to squeeze fluid into the urethra as sperm move through during sexual climax (ejaculation).
Prostatic fluid contains nutrients for the sperm, activates them and has other roles in sexual reproduction. The prostate provides much of the volume of the ejaculate.
Lower urinary tract symptoms (LUTS) attributed to benign prostatic obstruction (BPO) is a very common problem affecting the ageing male. The prevalence of LUTS in Europe varies with age, ranging from 14 percent in men in their 40’s to more than 40 percent in their 60’s. Assuming an overall prevalence of LUTS of 30 percent, this would mean that in the UK approximately 4 million men over the age of 40 years have LUTS.
One cause of obstruction can be from the prostate gland enlarging. As men age their prostate becomes enlarged and this condition is known as benign prostatic hyperplasia (BPH) the exact cause of which is unknown. The condition is associated with hormonal changes that occur as men age.
The testes produce the male hormone testosterone, which is converted to a more active form dihydrotestosterone (DHT). High levels of dihydrotestosterone are produced in the cells of the prostate and cause prostate growth ‘hyperplasia’ (enlargement). How and why levels of DHT increase remains a subject of research.
As the prostate gland grows it can squeeze the water pipe (urethra), or the neck of the bladder can be tight or enlarge. These can make it more difficult for the urine to flow freely and the bladder works harder to force urine through the narrowed waterpipe. This leads to the bladder wall becoming thicker and more sensitive, and makes it more difficult for the bladder to empty completely.

Those that occur during the filling of the bladder known as ‘storage symptoms’ and those that are present whilst urine is being passed are known as ‘voiding symptoms’
The main storage symptoms are:-
- Frequency – describes the number of times you go to the toilet during waking hours. For men it is usual to go 4 – 8 times, although of course this depends on how much you drink.
- Nocturia – means getting up at night to pass urine. This also becomes much more common as you get older and it is normal for men over 70 to get up at least once. This will again depend on the timing of your fluid intake.
- Urgency – a sudden strong feeling which tells you to “go now or you might leak urine”. This becomes more common as we get older.
- Incontinence – a medical term referring to the accidental leakage of urine. It can vary from a few drops to a flood. In older men, urge incontinence is the most common type seen. There is an urgent need to urinate but you leak before you can get to the toilet.
The main voiding symptoms are:-
- Decreased steam – the speed of flow of urine has decreased compared to when you were younger. This happens to all of us to some degree.
- Hesitancy – when you get to the bathroom and you are ready to pass urine, nothing happens for a few seconds or even longer.
- Intermittency – a medical term meaning to pass urine in a broken stop/start stream rather than a continuous one.
- Feeling of incomplete emptying – feeling that you still need to pass urine again even though you have just tried to empty your bladder.
- Dribbling – There are three types:
- Incontinence or wetness occurring at any time as the bladder fills.
- Terminal dribbling where the urine stream starts off reasonably strong, but slows to a dribble towards the end and therefore goes on and on.
- Post-micturition dribble, where you think you have finished, you dress yourself, walk away from the toilet and then lose some urine on to your clothes.
These different types of dribble have different causes and therefore different types of treatment.
The Causes of Nocturia may include:
- Excessive fluid intake before going to bed.
- Reduced bladder capacity. There is a tendency for bladder capacity to be reduced, as you get older. Bladder retraining can help but improvement at night will only come when any daytime problem has been dealt with.
- Having a different ‘body clock’, which causes a normal daytime pattern to occur at night.
- Diabetes, if it is not controlled. This leads to sugar appearing in the urine, which stimulates extra urine to be produced.
- If the bladder is unstable or irritated as a result of cystitis
- Swollen ankles and legs with excess fluid. At night when you lie down this excess fluid is reabsorbed into the blood stream and the kidneys then produce more urine.
BPH is rarely life threatening. However if left untreated it can lead to irreversible bladder or kidney damage.
The bladder can become distended and little blowouts form in the bladder wall - known as diverticulae; these may hold stale urine, which can then become infected. Backpressure may also be exerted onto the kidneys as the bladder is unable to empty, the bladder distends and that pressure rise can be transmitted back up to the kidneys.
Some men find they are suddenly unable to pass urine, empty their bladder and have severe pain and discomfort in the lower abdomen; this is referred to as Acute Urinary Retention (AUR).
If this situation occurs you need to attend a hospital’s emergency department to have a catheter inserted. A catheter is a slim plastic tube that is gently passed through the water pipe to drain urine away.
Other symptoms that can develop over time include Urinary Tract Infections (UTI’s) bladder stones and incontinence.
 Your GP or Consultant will refer you to a Prostate Assessment Clinic or a Lower Urinary Tract Symptoms (LUTS) clinic for an assessment. Your GP or Consultant will refer you to a Prostate Assessment Clinic or a Lower Urinary Tract Symptoms (LUTS) clinic for an assessment.
The Assessment
During the assessment a number of tests may be performed, these may include;
- A urine test to check for infection and blood.
- A digital rectal examination to feel if the prostate is enlarged and to check for any abnormalities.
- A urine flow test to check how fast you pass urine and record the volume.
- An ultrasound scan to check if any urine is left in the bladder after you have passed water.
- A blood test to assess how well the kidneys are working and a PSA blood test
Prostate Specific Antigen (PSA) is a substance produced in the prostate gland and detected in the blood therefore a blood test can be taken to measure the levels.
It is normal for men to have low levels of PSA in their blood; however, prostate cancer or benign (not cancerous) conditions can increase PSA levels. As men age, both benign prostate conditions and prostate cancer become more frequent. The most common benign prostate conditions are prostatitis (inflammation of the prostate) and benign prostatic hyperplasia (BPH) (enlargement of the prostate). There is no evidence that prostatitis or BPH cause cancer, but it is possible for a man to have one or both of these conditions and to develop prostate cancer as well.
PSA levels alone do not give doctors enough information to distinguish between benign prostate conditions and cancer.
However, PSA is not a specific test for cancer, and before you have the test you need to have discussed the implications of the results with your Doctor or Nurse Specialist.
You need to consider the following points carefully before you decide to have the test:
- A low PSA does not completely exclude prostate cancer.
- A high PSA does not mean there is prostate cancer, although the higher the PSA the greater the risk there is cancer.
- A high PSA can be due to simple benign enlargement of the prostate, which is very common in men over 50. It can occur during infection of the urine or the prostate, and after operations or tests on the prostate. The average level of PSA tends to be higher in older men.
If you have symptoms of bladder irritation, where you are going to the toilet very frequently or with some urgency, your consultant may ask that you have an investigation called bladder pressure studies, or Urodynamics.
This frequency and urgency is sometimes due to the bladder muscle having to work harder to get the urine past the prostate gland, and as a result the bladder continues to squeeze or spasm intermittently giving you the feeling that you need to empty your bladder frequently.
Urodynamics involves having a fine catheter passed via the water pipe into you bladder and a second fine catheter measuring the pressure of your tummy muscle just inside the back passage, the pressures in your bladder and tummy are measured as your bladder fills and empties. This test is important as it ensures that the doctors are able to give you the correct treatment for your condition.
Flexible cystoscopy
If you have severe irritative symptoms such as frequency, urgency, passing small volumes. Urine infections, or blood detected in your urine you will require a flexible cystoscopy.
The procedure is called a flexible cystoscopy, because a flexible instrument known as a cystoscope is used, which is inserted via the water-pipe (urethra) and allows your doctor to examine the urethra and inside of your bladder. It can also be used to assess the size of the prostate gland. It is performed using a local anaesthetic gel, the procedure takes approximately 10 – 15 minutes and you will be able to go home shortly after the procedure has finished; you should be able to resume normal activities, eg. Driving and work straight away.
The aim of treatment is to improve the flow of urine, reduce symptoms and provide a better quality of life.
Three main treatment options are available:
This is suitable for men with mild symptoms and may wish to try a period of watchful waiting as a first course of action.
Many men are quite happy to live with their symptoms once they have been reassured that they do not have prostate cancer. There are a number of things that men can try which may help reduce the severity of their symptoms.
Below are some of these lifestyle changes that some men have found helpful:
- Reduce the amount of fluid you drink in the evenings, and especially at night just before going to bed.
- Reduce the amount of tea and coffee you drink as the caffeine in these drinks can irritate the bladder as well as cause more urine to be produced. Decaffeinated products are widely available, but convert slowly to avoid withdrawal symptoms.
- Avoid getting constipated as a full bowel can also squeeze the urethra closed and make passing urine more difficult, and in some cases, can stop the flow of urine altogether.
- Stop smoking as the toxins pass out of your body in the urine so can irritate the bladder coating and may make some of the symptoms worse. Smoking can cause bladder cancer.
- Try not to take over the counter cold and sinus medications that contain decongestants or antihistamines. These medications can increase urinary symptoms.
- Bladder retraining techniques can involve;
‘Double voiding’ this is when you pass urine normally, and once you have finished go off and do something else for 5 – 10 minutes and then come back to the toilet and try again. This helps ensure that your bladder empties completely. This can be useful prior to going to bed to reduce the number of times you get up at night.
For frequency of passing urine try to hold the urge to pass urine for 5 minutes longer each time, until you reach a time period of 2½ hours between passing urine. You may find it helpful to keep a record chart.
Try one suggestion at a time to find out which lifestyle change is making a difference or not.
Medical management is most beneficial in people who have moderate symptoms, rather than mild or severe. Medical management involves using drugs to improve symptoms. These drug treatments are not a ‘cure’ and need to be taken for a long time.
There are two types of drug available. These are classed as:
- Alpha-blockers (relax the neck of the bladder and the prostate)
- 5 alpha-reductase inhibitors (reduce the size of the prostate)
Alpha-blockers
Alpha-blockers have been shown to increase urine flow-rates and improve symptoms associated with BPH and a tight bladder neck.
They work by causing the smooth muscle in the prostate and bladder neck to relax, which in turn relieves the obstruction and therefore increases the ability for urine to flow.
Types: The common alpha-blockers used are Alfuzosin, Doxazosin, Indoramin and Tamsulosin.
Improvement in symptoms is usually noticeable within a couple of weeks. If no improvement is noticed after a month then it may be worth you stopping these and considering an alternative treatment.
Side effects: The most common side effects from alpha-blockers may include headaches, tiredness, and dizziness in 10 –15 percent of patients. These are caused because this group of drugs also relax the blood vessels so that blood passes through them more easily which in turn lowers blood pressure.
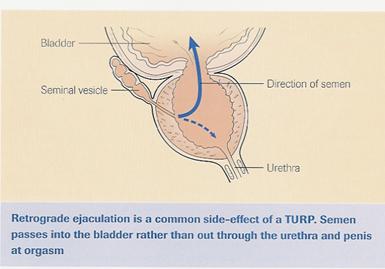
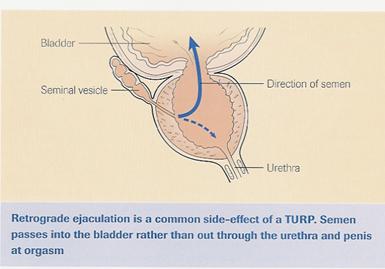
Retrograde ejaculation is where the semen goes back into the bladder when ejaculation occurs. This is not harmful, the next time you pee the urine may be cloudy.
5 alpha reductase inhibitors
Unlike alpha-blockers, 5 alpha reductase inhibitors can potentially slow the progression of BPH. This is because they work by interfering with the production of the enzyme (dihydrotestosterone), which is needed for the prostate to grow.
As a result the volume of the prostate reduces by about 25 percent after six months, which relieves the obstruction (caused by a narrowed waterpipe ‘urethra’) and the associated symptoms.
These tablets work better in men with larger prostates and shrinking may reverse the problem. Recent studies have shown that fewer patients then need operations for their prostate or experience the sudden inability to pass urine (acute retention).
When you have your PSA rechecked the result will be halved and therefore the result has to be doubled.
Types: There are two 5 alpha reductase drugs available, these are Finasteride and Dutasteride. It can take up to 6 months before you see improvement in your symptoms.
Side effects: Most of the side effects which can occur are usually reversed on stopping the treatment, but potential side effects include a loss of libido (sex drive), nipple and breast tenderness, erectile dysfunction and a reduction in the amount of ejaculate. However on the whole these drugs are well tolerated.
Your doctor or nurse specialist may suggest a combination therapy of both an alpha-blocker and a 5 alpha reductase.
These have been used in parts of Europe for many years and are becoming more popular in the UK. Many men who take herbal remedies say that their symptoms improve but no long-term studies have
been performed on these plant extracts. One such example of plant extract is Saw Palmetto these can be bought from a chemist or health food shop and are not available on prescription.
TUR(P) Trans Urethral Resection of Prostate has been the ‘gold standard’ in surgical treatment for many years, the latest advancement for surgery is using the high powered ‘Greenlight’ laser, this is known as PVP, Photoselective Vaporisation of the Prostate.
When the prostate is of a small volume, a Bladder Neck Incision may be preferred rather than a TURP.
These three surgical techniques are now explained below:
Bladder neck incision
No prostate tissue needs to be removed in this procedure. The results are often as effective as a TURP and with lower incidences of side-effects, however this is only suitable for men with small sized prostates.
TUR(P)
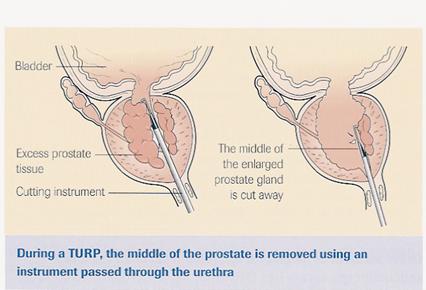
An instrument (resectoscope) is inserted via the water pipe (urethra) and through the prostate gland, into the bladder.
It has a telescope and light guide, which allows the Urologist to see inside the bladder and prostate. The operation is performed internally under direct vision.
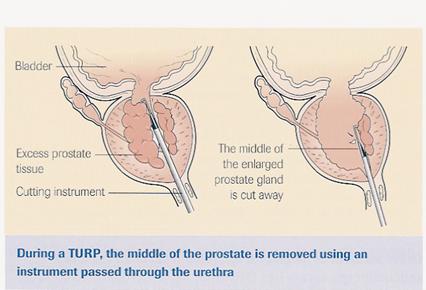
The resectoscope uses a wire loop to remove areas of tissue from the prostate that are blocking the urethra and allows blood vessels to be sealed (cauterised) to reduce the risk of bleeding afterwards.
TUR(P) is performed under anaesthetic. This may involve a general anaesthetic (asleep) or a spinal anaesthetic (awake but numb from the waist down).
This will be discussed with you beforehand. You should expect to stay in hospital for between 2 – 4 days, the procedure is minimally invasive and does not involve any external cuts.
All patients require a draining tube (catheter) to drain urine form the bladder after the operation.
 TUR(P) normally takes between 30 – 40 minutes to perform, although having an anaesthetic makes this time longer. The whole procedure takes about 60 minutes. TUR(P) normally takes between 30 – 40 minutes to perform, although having an anaesthetic makes this time longer. The whole procedure takes about 60 minutes.
Important points about TUR(P)
Any operation and anaesthetic carry risks, these are generally small and not doing the operation may carry a greater risk.
Risks of anaesthetic can be discussed with the anaesthetist who will be looking after you during the procedure and will normally visit you before the operation.
Retrograde Ejaculation – this occurs in nearly all men after TUR(P), i.e. rather than sperm being ejaculated out through the penis during sexual climax, the sperm pass back into the bladder and are passed out in the urine. This may reduce the ability to have children, but is NOT a means of contraception.
Urinary Catheter – it is sometimes necessary for men to be sent home with a catheter for a few weeks after the operation to allow the prostate to heal or rest the bladder for a period of time.
During this operation we will also look inside the bladder. Sometimes, we find bladder growths and stones, which may be treated during this operation.
Impotence – there is a reported risk (7-10%) of impotence after the operation. However, if men were unable to achieve an erection before the operation then having the operation will not improve this.
If this is a problem, treatments are available e.g. Viagra, Vacuum Devices.
Most men notice improvement in their symptoms within 6 weeks of the operation. However, in a few men it can take several months to notice an improvement in their symptoms.
Regrowth of the Prostate gland – because only the areas of prostate gland that are causing the obstruction are removed then the remaining gland may regrow and need a further operation, a number of years later. (up to 10%)
TUR(P) is usually performed for non-cancerous (benign) growth of the prostate gland, however tissue removed during the operation is sent for analysis to confirm that the areas removed were benign.
The results of this analysis (histology) will be discussed with you at the outpatient’s appointment after the operation.
Bleeding
Up to 4% of men having a TURP may require a blood transfusion. Bleeding may occur around the time of surgery or immediately after or it may restart once the bleeding appears to have settled. If this happens do not panic! Drink extra fluids (up to 3 litres per day) and rest. If the bleeding fails to settle contact the hospital (it is more likely if you strain or exert yourself during the first 2 weeks).
For the first 10-14 days at home you may well still experience some frequency and burning when passing urine.
You may continue to pass some blood in your urine too.
Some men experience an urgent need to pass urine (frequency) and discomfort when passing urine; these symptoms normally pass over the first couple of weeks at home.
There are a few sensible precautions to take when at home and would advise you not to
- Lift for 2-3 weeks
- Have sexual intercourse for 2 weeks
- Work for 1 week
- Drive for 2 weeks
These are guidelines only and should be discussed with your Doctor/Nurse before you go home.
PVP Photoselective Vaporisation of the Prostate
PVP is performed under anaesthetic. This may involve a general anaesthetic (asleep) or a spinal anaesthetic (awake but numb from the waist down.) This will be discussed with you beforehand.
As with a TURP an instrument known as a cystoscope is passed via the waterpipe (urethra), through the prostate gland and into the bladder.
The laser is passed through the cystoscope and on firing removes the tissue from the prostate and simultaneously seals the many blood vessels in the prostate.
As there is very little bleeding form the prostate after this procedure, a drainage tube from the bladder (a catheter) may or may not be required. Either way, you may be able to go home the same day (returning for removal of the catheter the following day) or stay one night in hospital.
Most men notice an improvement in their symptoms almost immediately after the operation. However, in a few men it can take several months to notice an improvement in their symptoms and in all men things continue to improve the first year or so.
Retrograde Ejaculation - this occurs in roughly 35% of men, i.e. rather than sperm being ejaculated out through the penis during sexual climax, the sperm pass back into the bladder and are passed out in the urine. This may reduce the ability to have children, but is NOT a means of contraception.
The incidence with this procedure is less than half that of a TURP.
Urinary catheter – it is rarely necessary for men to be sent home with a catheter for a few weeks after the operation to allow the prostate to heal or rest the bladder for a period of time.
During this operation we will also look inside the bladder.
Sometimes, we find bladder growths and stones, which may be treated during this operation.
Impotence – there is a very low risk of impotence after the operation, in fact there are no reported cases thus far, although the risk is unlikely to be nil. However, if men were unable to achieve an erection before the operation then having the operation will not improve this.
Redo operation – because only the areas of prostate gland that are causing the obstruction are removed, then the remaining gland may regrow and need a further operation a number of years later. As PVP is a relatively new technique we do not know what the risk of this is although we would estimate at 10% over 10 years.
Urinary Incontinence – there is a small risk (less than 1%) of men becoming incontinent of urine after the operation.
Urinary Tract Infection, (approx. 5% of patients) immediately after the operation or when at home, you will be given antibiotics at the time of surgery to reduce this risk.
Post Operative Recovery for TURP and PVP
After the operation you will normally “come round” in the recovery area, then be collected and taken back to the ward by a member of nursing staff once you are awake and comfortable.
Once back on the ward your blood pressure, pulse and temperature will be checked regularly and as soon as you feel able then you will be allowed to drink and eat.
If you have had a TURP performed it may be necessary to irrigate your bladder with saline (salty water) via the catheter that is in you bladder.
The catheter will stay in for 2- 3 days.
If you have had a PVP you may or may not return to the ward with a catheter. If you return with a catheter this will be removed a couple of hours later when you are awake, or left in overnight and removed first thing in the morning.
The recovery for PVP
- A small amount of blood may be seen in the urine for a few days after the procedure. Once this has settled down, at about 10 days to 3 weeks some patients describe some further blood at the start of the stream of urine. This has normally settled by 6 weeks.
- Some patients describe a mild burning sensation in the water-pipe, this usually settles within the first month.
- Formation of urethral stricture (a fibrous scar in the water pipe may form after such a procedure, this occurs in less than 1% of patients, but may require corrective surgery in the future.)
- Inability to pass urine after the catheter is removed (Retention of Urine) in up to 15% of patients. A catheter would be re-inserted and would stay in place for a number of weeks and you would be sent home with the catheter.
- Some men have the urge to pass urine, even when the catheter is in place, this can be caused by the catheter irritating the bladder lining. Tell a member of the nursing staff, as it is possible to give you medication to relieve this feeling.
Approximately 10-14 days after your operation it is common for you to pass some blood in your urine. It is important that you drink plenty (4 – 6 pints of fluid extra per day) to help “flush” the system through.
Recovery for PVP
Overall the recovery for PVP is significantly quicker than a TURP. Not only are you discharged quickly…BUT YOU RECOVER MORE QUICKLY TOO. Sexual activity is possible after 1 week and normal activity after 2 weeks.
Who should I contact for more information?
- The Specialist Urology Nurses:
- Sue Sill & Chris Backhouse
020 8934 3547
- Yvonne Haffenden, Lin Williams & Suzy Vallis
Urodynamics - 020 8934 3038
- The Urology Ward – Alexandra: 020 8934 3152
- If you have a known cancer condition and would like further information regarding this, please contact: Olga Champ - Clinical Nurse Specialist for Urology Oncology 020 8934 2729
Useful contacts:
www.greenlightlaser.com
www.urologypartners.co.uk
www.prostate-research.org.uk
If you think of any questions you wish to discuss at your next visit to the Urology Department, please record them below (to ensure you do not forget them)

When compared to the conventional open surgical technique, laparoscopic nephrectomy has resulted in significantly less post-operative pain, a shorter hospital stay, earlier return to work and daily activities, a more favourable cosmetic result and outcomes identical to that of open surgery.
Aspirin, lbuprofen, Alka Seltzer, Vitamin E and some other arthritis medications can cause bleeding and should be avoided 1 week prior to the date of surgery (Please contact your surgeon's office if you are unsure about which medications to stop prior to surgery. Do not stop any medication without contacting the prescribing doctor to get their approval).
This procedure has been performed on many patients over the last several years. Typically, the length of the operation is 3-4 hours. The surgery is performed through making 3 small (1cm) incisions in the abdomen. The kidney is usually removed by placing it within a bag and morcellating the kidney into pieces small enough to be removed through one of the incision sites. Incisions 2-3 inches in order to remove the kidney as an intact specimen
Although this procedure has proven to be very safe, as in any surgical procedure there are risks and potential complications. The safety and complication rates are similar when compared to the open surgery. Potential risks include:
Bleeding: Blood loss during this procedure is possible and a transfusion is needed in 5% of patients.
Infection: All patients are treated with intravenous antibiotics, prior to starting surgery to decrease the chance of infection from occurring after surgery. If you develop any signs or symptoms of infection after the surgery (fever, urinary frequency/discomfort, pain or anything that you may be concerned about) please contact us at once.
Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures,, spleen, liver, pancreas and gallbladder could require further surgery. Injury could occur to nerves or muscles related to positioning. Hernia at incision site is a possibility.
Hernia: Hernias at incision sites rarely occur since all keyhole incisions are closed under direct laparoscopic vision.
Conversion to Open Surgery: The surgical procedure may require conversion to the standard open operation if difficulty is encountered during the laparoscopic procedure. This could result in a larger standard open incision and possibly a longer recuperation period.
Immediately after the surgery you will be taken to the recovery room and transferred back to the ward once you are fully awake and your vital signs are stable.
Postoperative Pain: Pain medication can be controlled and delivered by the patient via an epidural or an intravenous infusion or by injection administered by the nursing staff. You may experience some minor transient shoulder pain (1-2 days) related to the gas used to inflate your abdomen during the laparoscopic surgery.
Nausea: You may experience some nausea related to the anaesthesia. Medication is available to treat persistent nausea.
Urinary Catheter: You can expect to have a urinary catheter draining your bladder (which is placed in the operating room while the patient is asleep) for approximately one day after the surgery. It is not uncommon to have blood-tinged urine for a few days after your surgery.
Diet: You can expect to have an intravenous infusion (IV) in for 1-2 days. (An IV is a small tube placed into your vein so that you can receive necessary fluids and stay well hydrated; in addition it provides a way to receive medication.) Most patients are able to tolerate ice chips and small sips of liquids the day of the surgery and regular food the next day. Once on a regular diet, pain medication will be taken by mouth instead of by injection.
Fatigue: Fatigue is common and should start to subside in a few weeks.
Hospital Stay: The length of hospital stay for most patients is approximately 2-3 days.
Constipation: You may experience sluggish bowels for several days or several weeks. Suppositories and stool softeners are usually given to help with this problem.
Pain Control: You can expect to have some incisional discomfort that may require pain medication for a few days after discharge.
Showering: You may shower at home. Your wound sites can get wet, but must be patted dry. Baths can soak your incisions and therefore are not recommended in the first 2 weeks after surgery. You will have adhesive strips across your incisions. They will fall off in approximately 5-7 days on their own. Sutures underneath the skin will dissolve in 4-6 weeks.
Activity: Taking walks is advised. Prolonged sitting or lying in bed should be avoided. Climbing stairs is possible. Driving should be avoided for at least 1- 2 weeks after surgery. Absolutely no heavy lifting (greater than 20 pounds) or exercising (jogging, swimming, treadmill, biking) for six weeks or until instructed by your doctor. Most patients return to full activity at home on an average of 3 weeks after surgery. You can expect to return to work in approximately 4 weeks.
|